Lower back pain treatment near me, san antonio chiropractor is a service that uses chiropractic care to relieve discomfort and restore mobility using natural methods. Our approach begins with spinal adjustments and manual therapy aimed at reducing pain quickly. Many people suffer from lower back pain due to muscle tension, poor posture, or sports injuries. At our clinic, we combine non-surgical treatments and first-hand experience with proven techniques to help you return to your daily activities pain-free. We believe in a data-driven strategy that focuses on long-term back health, offering clear guidance and practical methods for overcoming back discomfort today.

Understanding Your Pain And Exploring Treatment Options
If you sometimes feel a sharp or dull pain in your lower back, you are not alone. Many people look up lower back pain treatment near me or search for a san antonio chiropractor to get help. There are many reasons for lower back pain. It can happen because of muscle strain, posture issues, or sports injuries. Even everyday activities can lead to problems when the back is not cared for properly.
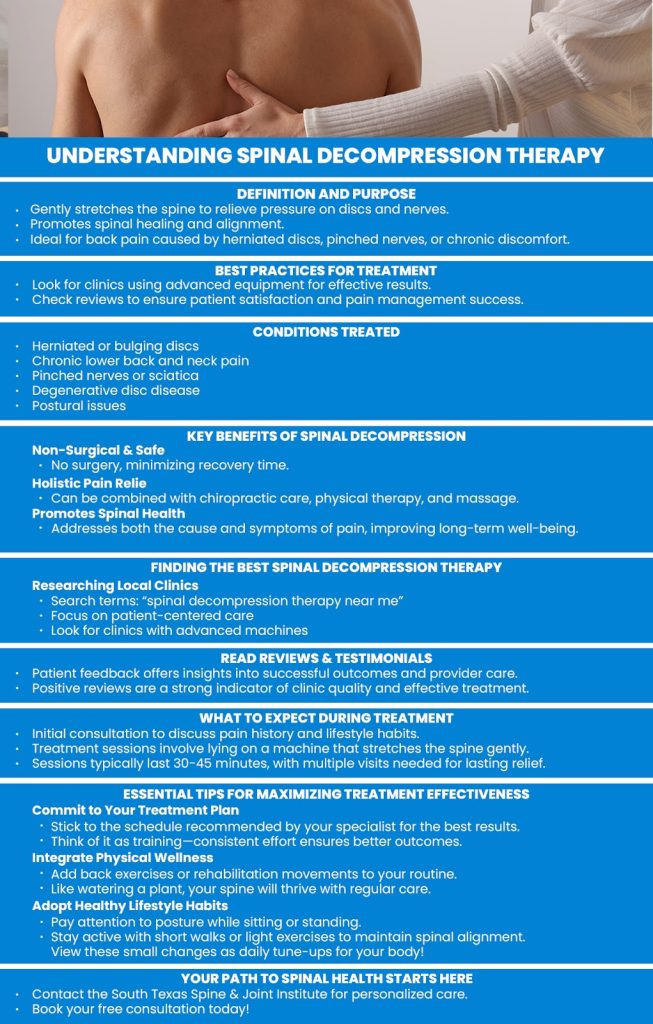
A mix of treatments can help reduce your pain. Some options are chiropractic care with a san antonio chiropractor, manual therapy, or physical therapy options. Others might get non-surgical treatment like chiropractic adjustments or natural pain relief. With personalized treatment plans, you can work with a back pain specialist to plan exercises and corrections that fit your life. With simple yet effective methods like posture correction, chiropractic adjustments, and manual therapy, you can start feeling better soon.
What Causes Lower Lumbar Pain?
Lower lumbar pain starts in the small muscles or the joints in your lower back. It happens when muscles get too tight or when the spine does not move correctly. Common reasons include muscle tension, spinal misalignment, and swelling in the back, which is often due to inflammation. For example, if you bend awkwardly at pick-up, you might injure a muscle. Other examples include sports injuries where your spine gets jolted, or long hours of sitting that lead to poor posture.
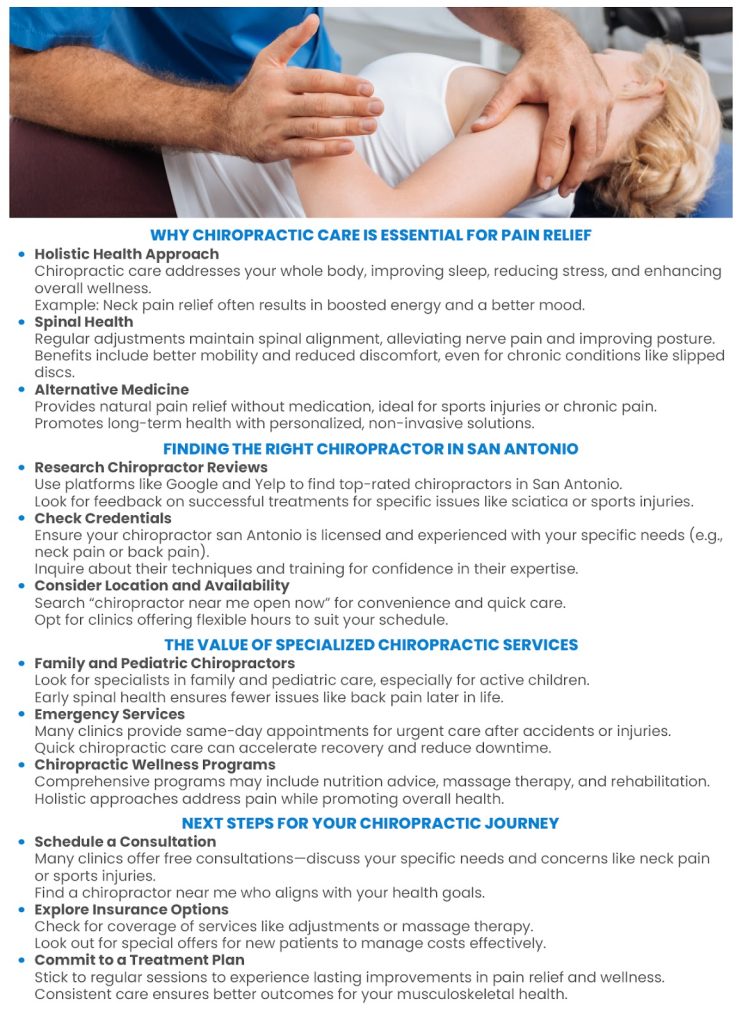
Many experts recommend chiropractic care to help fix these issues. A san antonio chiropractor can perform a chiropractic adjustment or use manual therapy to make movements easier and relieve pain. Simple, corrective exercises and posture correction methods are also effective. By focusing on spine health and back pain therapy, you can feel less pain and get back to your normal activities. With the right combination of chiropractic services and traditional physical exercises, lower back pain can gradually become less of a worry.
Innovative Approaches To Lower Back Pain Relief
Living with lower back pain can be hard. Many people search for lower back pain treatment near me or a san antonio chiropractor to feel better. New ideas and easy exercises can help you reduce pain quickly. Many experts believe that a mix of holistic back care and simple back pain exercises help your back feel strong again.
Alternative Pain Relief Strategies
A big part of feeling better is trying different approaches. Some doctors suggest chiropractic care that uses gentle spinal adjustment and manual therapy. These treatments work by easing muscle tension and improving spine health. For example, after a good chiropractic adjustment, many patients can move with less pain and enjoy everyday activities without worry.

A Customized Chiropractor Care Plan
A caring san antonio chiropractor can create a plan just for you. They may mix spinal decompression with back stabilization exercises to fix problems from an injury or everyday stress on the back muscles. Along with these treatments, simple lifestyle changes matter. A balanced diet, regular walking, and work breaks can add up to less pain over time. Everyone has a different body, so your plan could include pain management exercises, injury rehabilitation, and even manual manipulation. This plan gives you a chance to feel better without using medicines or surgery.
When looking for lower back pain relief or a back pain clinic, remember that a mix of care, exercise, and healthy habits works best. Your journey to a healthy back may start with one small step, like visiting a san antonio back pain relief center, and soon you can feel the comfort and care you deserve.
Data-Driven Results: The Impact Of Chiropractic Care In San Antonio
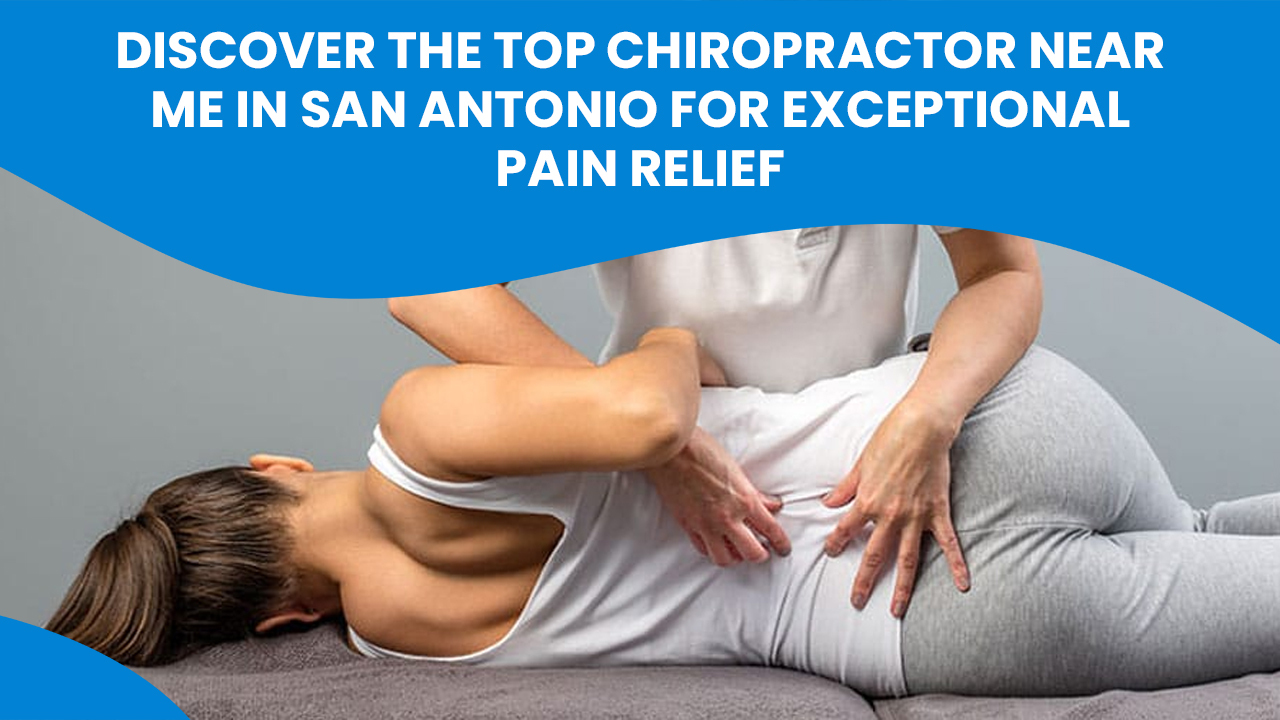
Chiropractic care in San Antonio has shown clear benefits for those seeking lower back pain treatment near me. Many patients report significant improvements in back pain relief after receiving spinal adjustment and manual therapy. Real-life case studies reveal quick recovery times, better spine alignment, and overall improved posture. For example, one patient shared that after several visits with a San Antonio chiropractor, his lower back pain decreased noticeably and he began doing simple back pain exercises that made a real difference in his daily life. These results are promising for anyone looking for a san antonio chiropractor who can offer affordable chiropractor options and a personalized treatment plan.
Real-World Outcomes With Spinal Adjustments
Data from local back pain clinics show that regular chiropractic adjustment sessions help reduce pain and improve back mobility. Patients often experience lower reliance on invasive procedures and report feeling better in a short time. Testimonials highlight that a mix of routine spinal adjustment techniques and back pain therapy can lead to: – Faster recovery from lower lumbar pain – Reduced muscle tension – Improved spine health and alignment
These real-world examples prove that integrating spinal adjustment into treatment plans can be very effective for lower back pain relief. Many people searching for treatment for lower back pain near their home have found success with these methods.
Integrating Manual Therapy And Correction Exercises
A combination of manual therapy, chiropractic adjustment techniques, and simple back pain exercises can further boost recovery. This method is supported by research that shows how blending hands-on care with gentle exercises helps reduce pain and correct posture issues. Here are some key points: – Manual therapy reduces pain quickly by easing tension in the muscles. – Chiropractic adjustments help realign the spine, improving spine alignment for better health. – Corrective exercises offer a way to maintain improvements after treatment and support overall mobility.
Together, these approaches provide a complete plan for back pain care. This improved technique is ideal for those seeking san antonio back pain relief as it combines alternative pain relief with practical, everyday movements. Choosing the right back pain clinic or consulting the best chiropractor san antonio recommends can set you on the path to lasting relief and recovery.

Wrapping Up Our Journey
After exploring these dynamic approaches to managing lower back pain, I feel more confident in my journey to recovery. My firsthand experience with chiropractic care and manual therapy at South Texas Spine & Joint Institute has helped me restore balance and reduce discomfort. I truly appreciate a strategy that mixes effective adjustments with simple back exercises. Living in San Antonio can be challenging, yet my improvements with spinal adjustments show meaningful progress. I invite you to consider a personalized plan that supports a healthier spine. Book your free consultation today by calling South Texas Spine & Joint Institute at (210) 545-7000 or emailing us, and let’s start your path toward lasting relief right now.